GMPコンプライアンス/バリデーションサービス
バリケア:GMP/GxPコンサルティングのプロフェッショナル
シンテゴングループのバリケアによるGMP(Good Manufacturing Practice)コンプライアンスサービスでは、特に製剤や原薬の製造、品質管理、保管、流通、売買など、GMP規制の対象となる分野で高度な専門知識を提供しています。経験豊富なGMPシニアコンサルタントが世界中の製薬・バイオテクノロジー・医療機器メーカーを対象に、ギャップ分析やコンプライアンス分析、基礎/専門トレーニング、標準コンサルティング、問題解決などでお客様をサポートします。また、リスクベースのクオリフィケーション、各種バリデーション(プロセス・洗浄・分析法・ITシステム)、GMPドキュメンテーションにおいても、生産能力に応じた実行サービスを提供しています。

バリケア ー 品質・GMPサービスのワンストッププロバイダー
バリケアはGMPコンプライアンス、クオリフィケーション・バリデーション、先端医療医薬品(ATMP)のGMPにおける理想的なパートナーとして、アドバイスの提供にとどまらず、ソリューションやプロセスの導入も行います。計画とプロジェクト管理から、実装およびドキュメンテーションまで、お客様のニーズやご要望に応じたサポートを行います。
GMPに準拠したプロジェクトのワークフローを設計・計画し、より包括的な工程やプロジェクトの仕様書(ユーザー要求仕様書:URS)を作成します。ここには、GMPプロジェクトの新規立上げや変更、再構築、是正処置/予防処置(CAPA)、包括的GMPまたは医薬品品質保証システムの確立・適用/最適化が含まれます。また、品質リスクマネジメント(QRM)、変更管理(CC)、逸脱管理(DC)、またはバリデーション戦略(プロセスバリデーション[PV]、洗浄バリデーション[CV]、方法バリデーション、分析法バリデーション[AMV]、コンピュータシステムバリデーション[CSV])など、GMP環境で必要とされる個々のコンセプトも記載します。
- GMPコンプライアンス関連事業で20年の実績
- 世界各国で2千件を超えるGMPプロジェクトの成功実績
- 学際的なチームがもつ幅広い能力
- 専門家によるGMPの実装と更新
- コンプライアンス分野で20年以上の経験をもつコンサルティング責任者
- 常にGMPコンプライアンス基準に関する最新の知識を提供
- 製薬・バイオテクノロジー・医療機器業界における分野横断的な事業
これらのサービスでは、事実を分析し、欠陥や逸脱、ギャップを発見します。ここでは製薬における古典的ツールであるGMP、ギャップ分析及び目標性能分析などを使用し、サービス対象にはGMP規制範囲のほか、GxPの領域全体、DIN EN ISO 9001:2015に基づく品質システム、DIN EN ISO 13485に基づく医療機器が含まれます。また、お客様のサプライヤー、委託検査機関や外部業者に対する第三者監査も実施します。ご要望に応じて、お客様のサプライヤーに対するクオリフィケーション全体を設計・計画し、代行します。
- 査察の重要ポイントを熟知した、有資格の監査担当者
- 規制について実地での経験豊かなGMPシニアコンサルタント
- GMPコンプライアンスについて外部から偏りのない視点を提供
- GMPコンプライアンス要件に関する最新の知識
バリケアは、シンテゴン製のシステムだけでなく、他社製のシステムに対してもクオリフィケーション・バリデーションサービスを提供しています。お客様のラボ用機器、滅菌機、バイオリアクター、発酵槽、ユーティリティーシステム、充填機、アイソレーターやクリーンルームなどを対象にクオリフィケーションを行います。さらに、既存システム、医薬品プロセス技術、充填・包装など、再クオリフィケーションの対象となる各システムのサポートも提供します。当社のクオリフィケーション範囲は常にリスクベースで決定されるため、不要なリソースの使用やコストの発生を回避することができます。当社のクオリフィケーションサービスは、EU GMPガイドラインのAnnex 15を含む国際的に有効なあらゆるGMPガイドラインに対応可能です。
- シンテゴンの子会社として、充填/プロセス技術についての知識が豊富
- 信頼性と柔軟性を兼ね備えた専門家集団がコスト効率の良いサポートを迅速に提供
- 確立された専門技術をもつ幅広い分野のエンジニア
- プロジェクトの計画・管理・実施における高い実践能力と効率性
バリケアは、プロセスバリデーション(PV)、洗浄バリデーション(CV)、分析法バリデーション(AMV)、コンピュータシステムバリデーションなど、製薬およびGMPの要件に基づく包括的なバリデーションサービスを提供しています。リスク分析からバリデーションプロトコルまで、また、試験仕様書からバリデーション報告書まで、あらゆるバリデーション活動に対応します。バリデーション文書には、それぞれのお客様との合意に基づいて決定した試験方法と判定基準を記載します。バリデーション結果を文書化し、規格への適合を確認します。さらに、逸脱に対して追跡調査、GMPに準拠した文書化、変更管理システムを通じた処理を行い、当社のバリデーションプロセスが完了します。
- シンテゴンの子会社として、充填/プロセス技術についての知識が豊富
- 信頼性と柔軟性を兼ね備えたエンジニアがコスト効率の良いサポートを迅速に提供
- 過去20年間に全世界で2000件を超えるクオリフィケーション・バリデーションプロジェクトの実績
- 高度な専門技術をもつ幅広い分野のエンジニア
- プロジェクトの管理と実施における高い実践能力と効率性
- 効率的な計画と実施により、製品上市までの期間を短縮
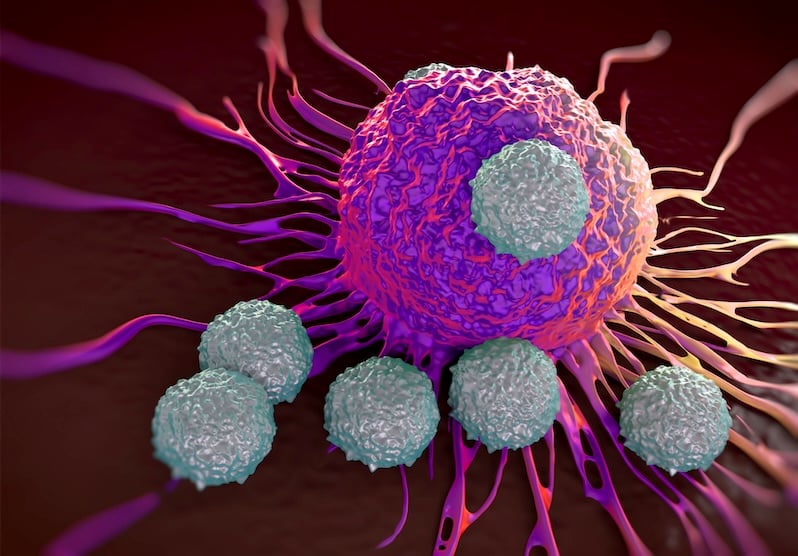
先端医療医薬品(ATMP)は個別化治療アプローチによってさまざまな病気を治療する可能性があります。ATMPの研究開発段階から、GMPに準拠した製剤の製造に至る過程の出発点は、多くの場合、臨床施設や小規模なスタートアップ企業です。この段階では、ATMPの製造はほとんど手作業により行われます。将来的にATMPが成功するためには、自動化プロセスへのスケールアップが不可欠です。当社はこの課題に取り組んでおり、ATMPのライフサイクル全体を通じてお客様をサポートします。
- 様々なATMP製造工程のGMPに関わる経験が豊富
- あらゆる工程とGMP規制要件に精通した専門スタッフ
- 製造と品質管理のコンセプトを速やかに構築
- 最新の医薬品品質管理システム(PQM)の要件に関する幅広い経験
- 医薬品開発における要求事項全般における経験
バリケアでは、ATMP向けサービスパッケージとして、GMP条件下における効率的なATMP製造工程の開発・移転・実施に対する専門的なアドバイスを提供します。通常のトレーニングサービス、ギャップ分析、第三者監査、サプライヤークオリフィケーション、リスクアセスメント、プロジェクト管理、クオリフィケーション・バリデーション、製剤開発、総合的なGMPドキュメンテーションの作成(管理下での保存を含む)により、お客様をサポートします。バリケアのcult.tainerはATMP向け一貫ソリューションであり、無菌プロセスの開発とATMPの製造を行う機器を完備したGMP準拠のクリーンルームモジュールです。GMPに関わるあらゆる問題について助言とサポートも含まれます。
- ATMP製造のリスクアセスメントにおけるGMPの豊富な経験
- あらゆる工程とGMP規制要件に精通した専門スタッフ
- サプライヤーのクオリフィケーション要件に関する豊富な実績
- 設備の設計・構築の要件に関する幅広い経験
- ATMP関連のワンストッププロバイダーとしてのバリケア
医薬品製造におけるGMPコンプライアンス

GMP/GDP training GMP/GDPトレーニング
当社では、GMP、GDP、クオリフィケーション・バリデーション、クオリフィケーションプロジェクトの計画、ATMP-GMP、医療機器、分析法バリデーション、ITシステムのバリデーション、リスク分析・リスク管理など、需要の多い標準/基礎トレーニングコースを数多く提供しています。さらに、指定されたテーマについてカスタマイズしたトレーニングコースをお客様施設で実施することも可能です。また、バーチャルトレーニングの実施やドイツ・フランクフルトの当社施設でトレーニング実施も可能です。

コンピュータシステムバリデーション(CSV)
お客様の設備が既存のシステムであるか立上げ前のシステムであるかを問わず、GLP(Good Laboratory Practice)、GCP(Good Clinical Practice)、GMP(Good Manufacturing Practice)、GDP(Good Distribution Practice)と医療機器におけるコンピュータシステムバリデーション(CSV)の要件への対応をサポートします。当社では、国際製薬技術協会(ISPE)の "Good Automated Manufacturing Practice 5" (GAMP 5)に基づいて実装を行います。私たちは幅広いカテゴリーのソフトウェア・ハードウェアのバリデーションに精通しています。また、一般的なITアプリケーションのバリデーションについても実施予定です。

ATMP製造設備
現状のATMP製造では、依然として個別化アプローチ(患者1名に1製品)が採用されており、自動化や大規模スケールでの生産には至っていません。このような状況のもと、バリケアはその親会社であるシンテゴンと協力して、モジュール設計/構造で簡単に実装できる新しいクリーンルームレイアウトのコンセプトを確立しました(valicare.tainer)。この柔軟なコンセプトにより、出発原料から治験用ATMP製品(iATMP)まで、GMPに準拠した開発と製造が可能になります。個別の要件に合わせてGMP対応クリーンルームモジュールを構築し、ターンキーソリューションとして提供することが可能です。

ドキュメンテーションのエキスパート
バリケアは長年にわたり、GMPに準拠した製品ライフサイクルで必要となる文書のテンプレートを作成してきました。品質やコンプライアンスの制限を受けることなく、より迅速な対応が可能です。詳しくはバリケアのウェブサイトをご覧ください!
関連情報
「持続可能性、効率性、デジタル化、安全性、柔軟性」は、産業における重要なトレンドです。 私たちは自社の技術やノウハウを活用して、これらの課題に対する解決策を開発し、未来の製造業を形作っています。
Frequently asked questions
Compliance in pharmaceutical industry mainly refers to GMP compliance, meaning compliance with current legally binding pharmaceutical quality system requirements as outlined in worldwide aligned GMP regulations.
Regulatory compliance requires companies to fulfill all legally binding prerequisites given by a respective drug law to guarantee quality, safety and efficacy of a drug product, as described e.g. in international standards and national laws.
Regulatory compliance is ensured by covering all regulatory requirements referring to the market authorization of a drug product for a specific pharmaceutical market. General guidance on those requirements, arising from with manufacturing license, clinical trial authorization, drug registration and manufacturing authorization, can be found on the homepage of the ICH (International Council of Harmonization of Technical Requirements for Pharmaceutical for Human Use).
Process validation is the documented evidence that a manufacturing process leads to a pharmaceutical product of reproducible quality with pre-defined specifications.
Cleaning validation is the documented evidence that a reproducible cleaning process leads to a predefined reduction of contaminants and is mandatory for multipurpose process equipment.
Analytical method validation (AMV) is the documented evidence that an analytical method is suitable for intended use within pre-defined ranges. The internationally accepted common standard for AMV in the pharmaceutical industry is the ICH Q2(R1).
Regulatory compliance is monitored, for example, as part of inspections by the authorities. The medicinal product manufacturer is obliged to implement a PQS (pharmaceutical quality system) to follow and monitor the regulatory and GMP compliance. The PQS must be comprehensively documented using instructions. It records and includes all aspects that affect the quality as well as safety and efficacy of the medicinal product. The implemented quality system covers the entire lifecycle of the medicinal product from pharmaceutical development through technology transfer to commercial production until the product is discontinued. The quality tools, ongoing reviews, and verification as well as qualification of equipment, maintenance and validation of processes are some examples of monitoring regulatory compliance all covered by pharmaceutical quality assurance.
The regulation of pharmaceuticals provides the legal basis for quality, safety and efficacy of products which cannot obviously be evaluated by the end-user. The manufacturer of medicinal products should produce reproducible products in terms of quality attributes by means of validated production processes for the intended use with the main objective of patient safety. All processes and phases, from pharmaceutical development through technology transfer to commercial production until the product is discontinued, are regulated by the directives of authorities worldwide to achieve the safety of end users (patients).
Compliance with the regulated requirements (e.g. by EMA, FDA) is monitored via an implemented quality system, which is established to manage the company quality policies, procedures, and processes, as well as continuous improvement. The pharmaceutical quality system assures that the desired product quality is routinely met, and suitable process performance is achieved. The evidence of conformity is provided e.g. by procedures, protocols and linked documents for all operational processes from material acquisition, production, and testing to storage, import/export and market placement.
GMP data are generated, acquired, or collected as part of the GMP manufacturing site, clinical trials or development. This includes activities such as equipment and facility qualification and process and analytical method validation, raw and derived data as electronic documentation systems and paper-based documentation.
Prospective validation are the validation activities carried out before routine production of products intended for sale. Once the process is validated, the produced batches can be launched for sale.
Third-party audits are audits conducted by an independent third-party expert company, which was appointed by a pharmaceutical manufacturer) to inspect a supplier (auditee), e.g. as part of the supplier qualification of raw material, intermediate product, active pharmaceutical ingredient and excipient manufacturers, as well as equipment vendors, contract manufacturers, contract laboratories and service providers. The key component of a third-party audit is the independence of the audit company, which must be free of any conflict of interest.
Medicinal products are regulated by GMP guidelines. These are based on international standards and regional or national laws. In the U.S., pharmaceutical products are regulated by Title 21 of the Code of Federal Regulations (CFR), in the EU by the EU-GMP guideline, and by local guidelines in other countries.
These guidelines include requirements regarding pharmaceutical quality management (PQM), personnel, premises, equipment and procedures in manufacturing, quality control and product release, as well as outsourced activities. In addition, there are requirements for inspection and for handling deviations and complaints.
Since 2015, the International Council of Harmonization of Technical Requirements for Pharmaceutical for Human Use (ICH) began with the task of globally harmonizing regulatory pharmaceutical requirements. The alignment of the guidelines is ongoing.
Medical devices are regulated by the FDA in different CFRs (Code of Federal Regulation), e.g. 21 CFR 820 for quality management and European Medical Device regulation EC 745/2017 (MDR), mandatory since 05/2021. Many requirements seem similar to those for medicinal products, but this mainly concerns the continuous risk and quality management, the complete traceability and the consideration of the entire product life cycle. Additionally, a person (PRRC) is personally responsible for ensuring regulatory requirement and compliance.
To bring a medical device to the market, a Notified Body must be appointed to inspect and approve all technical and developmental documentation, risk assessment and measures focused on patient’s safety. This also includes the requirements for clinical evaluation and post-market surveillance.
In the pharmaceutical environment, the use of good practices is mandatory. The most prominent procedures are to be found in manufacturing (GMP), distribution (GDP), and documentation (GDocP). This type of abbreviation is also commonly used in clinical practice (GCP), in laboratory work (GLP), in automated manufacturing (GAMP) and in pharmacovigilance (GVP). The European Medicines Agency (EMA) provides guidelines for defining and safeguarding these practices. In the U.S., the FDA provides similar guidelines.
GxP stands for Good ‘X’ Practice where ‘X’ is used as a collective term for the middle noun:
- GDP – Good Distribution Practice
- GCP – Good Clinical Practice
- GLP – Good Laboratory Practice
- GMP (or cGMP) – Good Manufacturing Practice or current Good Manufacturing Practice
- GPvP – Good Pharmacovigilance Practice
- GDocP – Good Documentation Practice
- GEP – Good Engineering Practice
- GAMP – Good Automated Manufacturing
In case of advanced medicinal products of biological origin, the GMP requirements are adjusted to the products’ special demands, especially in the U.S. and in the EU. These products are defined in the U.S. as “of biological origin” and in Europe as “Advanced Therapy Medicinal Products” (ATMP). These products are mostly applied in special individualized therapies.
In contrast to the classical pharmaceutical industry, alternative manufacturing and quality control approaches are allowed, if the modifications follow the risk-based approach, are traceable and guarantee quality, safety, and efficacy of the product. Therefore, special instructions and requirements have been added to the guidelines.
Clear details on regulatory supervision and approvals can only be given for the U.S. and the EU; the Asia-Pacific region has no harmonized regulatory framework. Although China is ranking high in global advanced therapy clinical trials, their Drug Regulatory Action Plan (2019) and special guidelines are relatively young and not internationally harmonized.
Legal framework in the U.S. is profoundly established. For biological medical products, it is provided by section 351 of the Public Health Service Act (PHSA) and the Food and Drug Administration Act (FDCA), in detail by 21 CFR 600-680 and 1271.
In the EU, regulation EC No. 1394/2007 is binding for all ATMPs, which are therapeutically applied (in either case studies, clinical trials, or routine healthcare). They require at least a manufacturing authorization assigned by local authorities. Clinical trials are subject to the respective national authorities where the clinical trial is done. The application of the central European marketing authorization must be submitted to the European Medicines Agency (EMA).
In the U.S., the Food and Drug Administration (FDA) is responsible for regulation and approval. Application is under control of the Centre of Biological Evaluation and Research (CBER) and the Office of Tissue and Advanced Therapies (OTAT).
In the EU, the European Medicines Agency (EMA) regulates and approves ATMPs. EC 1394/2007 defined a Committee for Advanced Therapies (CAT), which reviews all inquiries based on a single evaluation and authorization procedure. The Committee for Human Medicinal Products (CHMP) has special working groups to support the CAT in risk assessment, scientific advice, and support of pharmacovigilance of ATMPs. Application in clinical trials is under control of national authorities. Since 2010, the so-called Voluntary Harmonization Procedure (VHP) can be applied using a simplified approval procedure. Here, a lead evaluating authority of a member state (as rapporteur) is given the opportunity to involve other member states in this approval.